Cervical Radiculopathy
Introduction
Physical therapy in Pittsburgh for Upper Back and Neck
Welcome to Greater Pittsburgh Physical Therapy & Sports Medicine's patient resource about Cervical Radiculopathy.
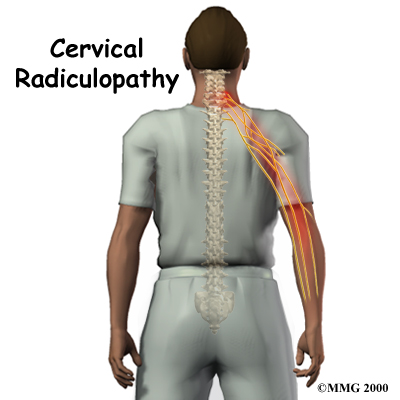
Neck pain has many causes. Mechanical neck pain comes from injury or inflammation in the soft tissues of the neck. This is much different and less concerning than symptoms that come from pressure on the nerve roots as they exit the spinal column. People sometimes refer to this problem as a pinched nerve. Health care providers call it cervical radiculopathy.
This guide will help you understand:
- how the problem develops
- how doctors diagnose the condition
- what treatment options are available
Anatomy
What part of the neck is involved?
The spine is made of a column of bones. Each bone, or vertebra, is formed by a round block of bone, called a vertebral body. A bony ring attaches to the back of the vertebral body. When the vertebra bones are stacked on top of each other, the bony rings forms a long bony tube that surrounds and protects the spinal cord as it passes through the spine.
Spine
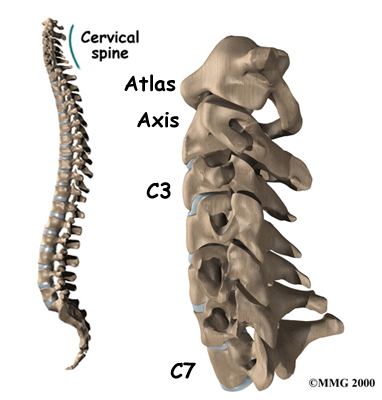
Bony Ring Surrounding Spine
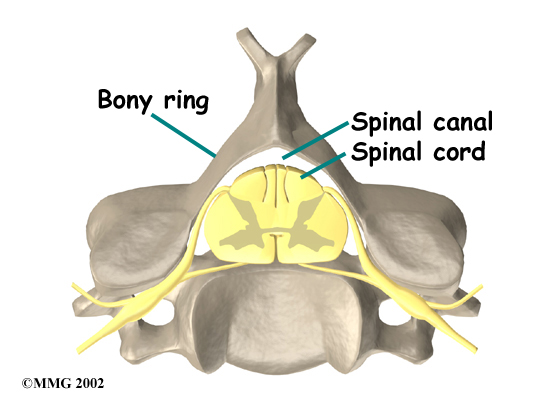
Travelling from the brain down through the spinal column, the spinal cord sends out nerve branches through openings on both sides of each vertebra. These openings are called the neural foramina. (The term used to describe a single opening is foramen.)
Foramen
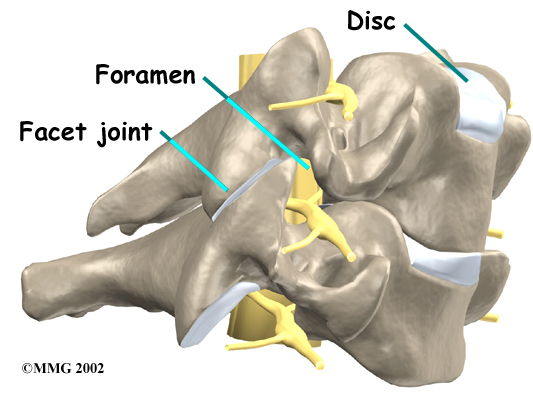
The intervertebral disc sits directly in front of the opening. A bulged or herniated disc can narrow the opening and put pressure on the nerve. A facet joint sits in back of the foramen. Bone spurs that form on the facet joint can project into the tunnel, narrowing the hole and pinching the nerve.
Herniated Disc
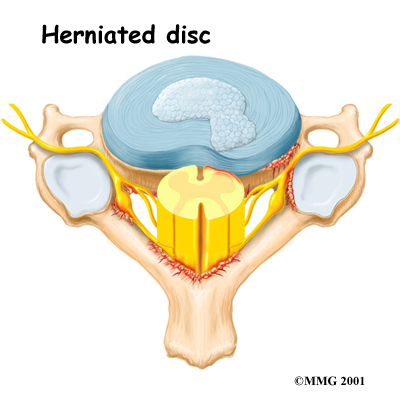
An intervertebral disc fits between the vertebral bodies and provides a space between the spine bones. The disc normally works like a shock absorber. An intervertebral disc is made of two parts. The center, called the nucleus, is spongy. It provides most of the shock absorption. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it. Ligaments are strong connective tissues that attach bones to other bones.
Causes
Why do I have this problem?
Cervical radiculopathy is caused by any condition that puts pressure on the nerves where they leave the spinal column. This is much different than mechanical neck pain. Mechanical neck pain is caused by injury or inflammation in the soft tissues of the neck, such as the discs, facet joints, ligaments, or muscles.
The main causes of cervical radiculopathy include degeneration, disc herniation, and spinal instability.
Degeneration
As the spine ages, several changes occur in the bones and soft tissues. The disc loses its water content and begins to collapse, causing the space between the vertebrae to narrow. The added pressure may irritate and inflame the facet joints, causing them to become enlarged. When this happens, the enlarged joints can press against the nerves going to the arm as they try to squeeze through the neural foramina. Degeneration can also cause bone spurs to develop. Bone spurs may put pressure on nerves and produce symptoms of cervical radiculopathy.
Herniated Disc
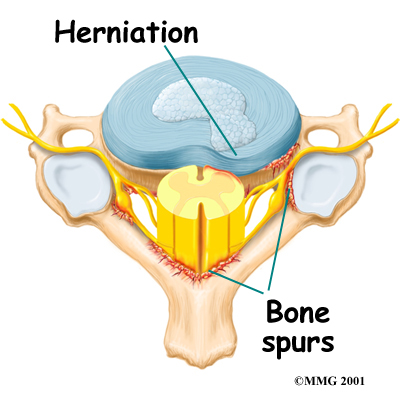 Heavy, repetitive bending, twisting, and lifting can place extra pressure on the shock-absorbing nucleus of the disc. A blow to the head and neck can also cause extra pressure on the nucleus. If great enough, this increased pressure can injure the annulus (the tough, outer ring of the disc). If the annulus ruptures, or tears, the material in the nucleus can squeeze out of the disc. This is called a herniation.
Heavy, repetitive bending, twisting, and lifting can place extra pressure on the shock-absorbing nucleus of the disc. A blow to the head and neck can also cause extra pressure on the nucleus. If great enough, this increased pressure can injure the annulus (the tough, outer ring of the disc). If the annulus ruptures, or tears, the material in the nucleus can squeeze out of the disc. This is called a herniation.
Although daily activities may cause the nucleus to press against the annulus, the body is normally able to withstand these pressures. However, as the annulus ages, it tends to crack and tear. It is repaired with scar tissue. Over time, the annulus becomes weakened, and the disc can more easily herniate through the damaged annulus. If the herniated disc material presses against a nerve root it can cause pain, numbness, and weakness in the area the nerve supplies.
Spinal instability
Spinal instability means there is extra movement among the bones of the spine. Instability in the cervical spine (the neck) can develop if the supporting ligaments have been stretched or torn from a severe injury to the head or neck. People with diseases that loosen their connective tissue may also have spinal instability. Spinal instability also includes conditions in which a vertebral body slips over the one just below it. When the vertebral body slips too far forward, the condition is called spondylolisthesis. Whatever the cause, extra movement in the bones of the spine can irritate or put pressure on the nerves of the neck, causing symptoms of cervical radiculopathy.
Symptoms
What does the condition feel like?
The symptoms from cervical radiculopathy are from pressure on an irritated nerve. These symptoms are not the same as those that come from mechanical neck pain. Mechanical neck pain usually starts in the neck and may spread to include the upper back or shoulder. It rarely extends below the shoulder. Headaches are also a common complaint of both radiculopathy and mechanical neck pain.
Pressure on Irritated Nerve
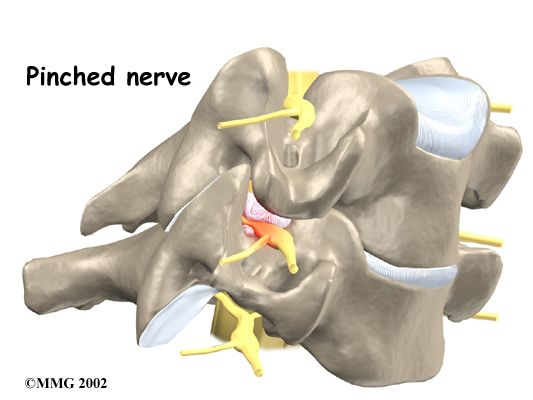
The pain from cervical radiculopathy usually spreads further down the arm than mechanical neck pain. And unlike mechanical pain, radiculopathy also usually involves other changes in how the nerves work such as numbness, tingling, and weakness in the muscles of the shoulder, arm, or hand. With cervical radiculopathy, the reflexes in the muscles of the upper arm are usually affected. This is why doctors check reflexes when people have symptoms of cervical radiculopathy.
Diagnosis
How do health care providers diagnose the problem?
At Greater Pittsburgh Physical Therapy & Sports Medicine, we gather the information about your symptoms as a way to determine which nerve is having problems. Diagnosis begins with a complete history of the problem. Our physical therapists will ask questions about your symptoms and how your problem is affecting your daily activities. Your answers can help us determine which nerve is causing problems.
Next, our physical therapist examines you to see which neck movements cause pain or other symptoms. Your skin sensation, muscle strength, and reflexes are tested in order to tell where the nerve problem is coming from.
Some patients may be referred to a doctor for further diagnosis. Once your diagnostic examination is complete, the physical therapists at Greater Pittsburgh Physical Therapy & Sports Medicine have treatment options that will help speed your recovery, so that you can more quickly return to your active lifestyle.
Greater Pittsburgh Physical Therapy & Sports Medicine provides services for physical therapy in Pittsburgh.
Our Treatment
Non-surgical Rehabilitation
Unless the nerve problem is getting worse rapidly, therapy usually begins with nonsurgical treatments. At Greater Pittsburgh Physical Therapy & Sports Medicine, Cervical Radiculopathy patients are normally seen a few times each week for one to two months. In severe cases, patients may need a few additional weeks of care. Our therapist will create a program to help you regain neck and arm function.
At first, treatments are used to ease pain and inflammation and may include immobilization devices and electrical stimulation treatments to help calm muscle spasm and control pain.
When you begin physical therapy at Greater Pittsburgh Physical Therapy & Sports Medicine, we may prescribe immobilization of the neck. Keeping the neck still for a short time can calm inflammation and pain. This might include one to two days of bed rest and the use of a soft neck collar . This collar is a padded ring that wraps around the neck and is held in place by a Velcro strap. Normally, a patient need only wear a collar for one to two weeks. Wearing it longer tends to weaken the neck muscles.
Soft Neck Collar

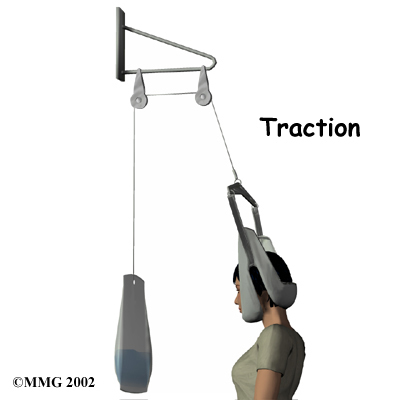
Treatments for cervical radiculopathy often include neck traction. Traction is a way to gently stretch the joints and muscles of the neck. It can be done using a machine with a special head halter, or the physical therapist can apply the traction pull by hand. Though neck traction is often done in our clinic, we may give you a traction device to use at home.
Special Head Halter
It is very important to improve the strength and coordination in the neck and shoulder blade muscles. Our therapist can also evaluate your workstation or the way you use your body when you do your activities and suggest changes to avoid further problems.
At Greater Pittsburgh Physical Therapy & Sports Medicine, we usually have their patients try nonoperative treatments for at least three months before considering surgery. But when patients simply aren't getting better, or if the problem is becoming more severe, we may refer you to a surgeon for evaluation.
Post-surgical Rehabilitation
Rehabilitation after surgery for cervical radiculopathy can be a slow process. Although recovery time is different for each individual, you may need to attend physical therapy sessions at Greater Pittsburgh Physical Therapy & Sports Medicine for six to eight weeks, and you should expect full recovery to take up to four months.
During physical therapy after surgery, our physical therapist may use treatments such as heat or ice, electrical stimulation, massage, and ultrasound to help calm pain and muscle spasm. Then we will begin to teach you how to move safely with the least strain on your healing neck.
As your Greater Pittsburgh Physical Therapy & Sports Medicine rehabilitation program evolves, you will do more challenging exercises. The goal is to safely advance your strength and function. As your physical therapy sessions come to an end, our therapist will help you with decisions about getting you back to work. We can do a work assessment to make sure you'll be able to do your job safely. Our physical therapist may suggest changes that could help you work safely, with less chance of reinjuring your neck.

When your treatment is well under way, your regular visits to Greater Pittsburgh Physical Therapy & Sports Medicine will end. We will continue to be a resource for you but you will be in charge of doing your exercises as part of an ongoing home program.
Greater Pittsburgh Physical Therapy & Sports Medicine provides physical therapy in Pittsburgh.
Portions of this document copyright MMG, LLC.
Physician Review
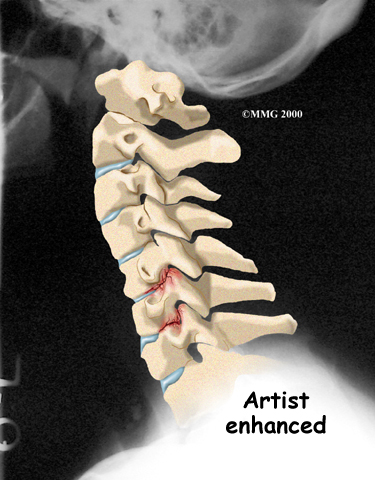
Your physician may order X-rays of the cervical spine to identify the cause of pressure on the nerve. The images show whether degeneration has caused the space between the vertebrae to collapse. They may also show if a bone spur is pressing against a nerve.
If more information is needed, your doctor may order magnetic resonance imaging (MRI). The MRI machine uses magnetic waves rather than X-rays to show the soft tissues of the body. This test gives a clear picture of the discs, nerves, and other soft tissues in the neck. The machine creates pictures that look like slices of the area your doctor is interested in. The test does not require any special dye or needles and is painless.
Sometimes it isn't clear where the nerve pressure is coming from. Symptoms of numbness or weakness can also happen when the nerve is being pinched or injured at other points along its path. (An example of this is pressure on the median nerve in the wrist, known as carpal tunnel syndrome.) Electrical studies of the nerves going from the neck to the arm may be requested by your doctor to see whether the nerve problem is in the neck or further down the arm. However, most doctors take X-rays and try other forms of treatment before ordering electrical tests. These tests are usually only needed when the diagnosis is not clear.
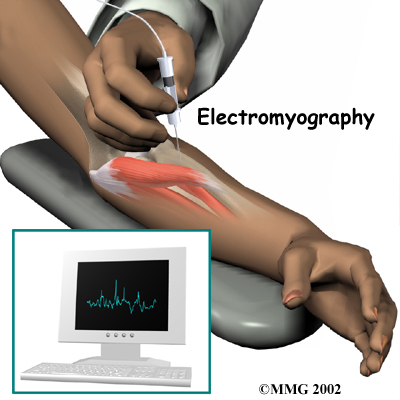 If your doctor orders electrical studies, several tests are available to see how well the nerves are functioning, including the electromyography (EMG) test. This test measures how long it takes a muscle to work once a nerve signals it to move. The time it takes will be slower if nerve pressure from radiculopathy has affected the strength of the muscle.
If your doctor orders electrical studies, several tests are available to see how well the nerves are functioning, including the electromyography (EMG) test. This test measures how long it takes a muscle to work once a nerve signals it to move. The time it takes will be slower if nerve pressure from radiculopathy has affected the strength of the muscle.
Another electrical test that may be used instead of EMG is cervical root stimulation (CRS). This test involves putting a small needle through the back of the neck into the nerve where it leaves the spinal column. Readings of muscle action are then taken of the muscles on the front and back of the upper arm and along the inside of the lower arm. Doctors use the readings to determine which nerve is having problems.
Doctors prescribe certain types of medication for patients with cervical radiculopathy. Severe symptoms may be treated with narcotic drugs, such as codeine or morphine. But these drugs should only be used for the first few days or weeks after problems with radiculopathy start because they are addictive when used too much or improperly. Muscle relaxants may be prescribed to calm neck muscles that are in spasm. You may be prescribed anti-inflammatory medications such as aspirin or ibuprofen.
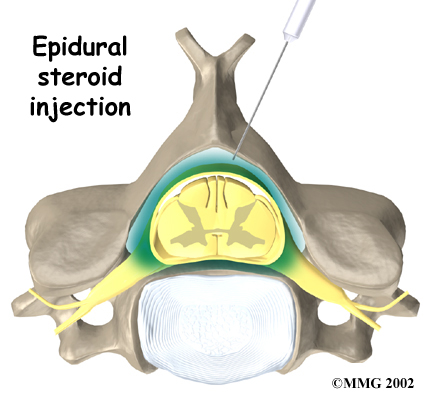
Some patients are given an epidural steroid injection (ESI). The spinal cord travels in a tube within the bones of the spinal canal. The cord is covered by a material called dura. The space between the dura and the spinal column is the epidural space. It is thought that injecting steroid medication into this space fights inflammation around the nerves, the discs, and the facet joints. In some cases, the steroid injection is given around one specific nerve. This is called a selective nerve block. The response to this treatment helps confirm which nerve root is causing the symptoms.
Epidural Steroid Injection (ESI)
Surgery
 Most people with cervical radiculopathy get better without surgery. In rare cases, people don't get relief with nonsurgical treatments. They may require surgery. There are several types of surgery for cervical radiculopathy. These include
Most people with cervical radiculopathy get better without surgery. In rare cases, people don't get relief with nonsurgical treatments. They may require surgery. There are several types of surgery for cervical radiculopathy. These include
- foraminotomy
- discectomy
- fusion
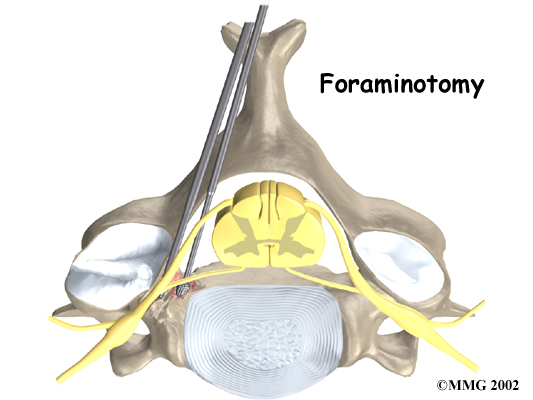
Foraminotomy
A foraminotomy is done to open the neural foramen and relieve pressure on the spinal nerve root. A foraminotomy may be done because of bone spurs or inflammation.
Related Document: Greater Pittsburgh Physical Therapy & Sports Medicine's Guide to Cervical Foraminotomy
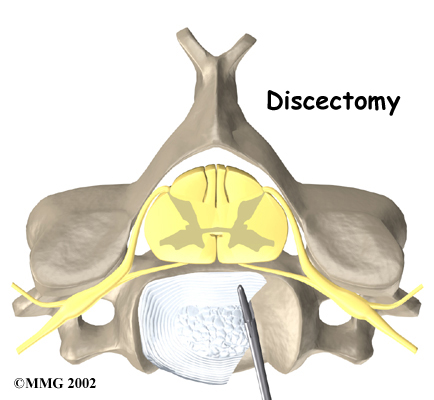
Discectomy
In a discectomy, the surgeon removes the disc where it is pressing against a nerve. Surgeons usually perform this surgery from the front (anterior)of the neck. This procedure is called anterior cervical discectomy. In most patients, discectomy is done together with a procedure called cervical fusion, which is described next.
Anterior Cervical Discectomy
Fusion
A fusion surgery joins two or more bones into one solid bone. The purpose for treating cervical radiculopathy with fusion is to increase the space between the vertebrae, taking pressure off the nerve. The surgery is most often done through the front of the neck. After taking out the disc (discectomy), the disc space is filled in with a small block of bone graft. The bone is allowed to heal, fusing the two vertebrae into one solid bone. The space between the vertebrae is propped and held open by the bone graft, which enlarges the neural foramina, taking pressure off the nerve roots.
Bone Graft
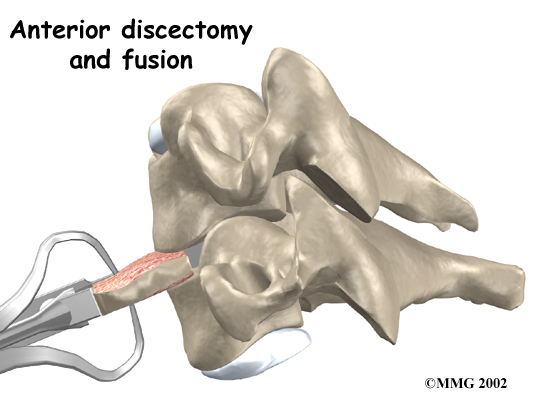
Related Document: Greater Pittsburgh Physical Therapy & Sports Medicine's Guide to Anterior Cervical Discectomy and Fusion
Portions of this document copyright MMG, LLC.